Maybe you are, but then again, maybe you’re not. Errors and omissions (E&O) policies cover things a company does, a company does not do, or that don’t turn out as a customer expected. Directors and officers (D&O) insurance policies provide protection for a company’s directors and officers whose personal financial assets can be put at risk in the event of a lawsuit. There are no standard D&O/E&O policies. Each insurer drafts its own version, and many fail to provide coverage in key areas. If the unfortunate happens and you become the target of a lawsuit, you don’t want to risk losing precious corporate – or personal – financial resources because of inadequate or inappropriate insurance coverage.
As part of our continuing effort to find ways to service you, Summit Re has entered into an arrangement with a national firm that specializes in property and casualty insurance products that are designed for organizations in the health care industry. This alliance was formed to help health plans gain access to better D&O and E&O policies. As part of this arrangement, we are able to offer you a complimentary analysis of your current coverage. A recent study showed that over 50% of directors and officers requested changes in their insurance coverage when they learned what was NOT covered under their current programs.
To perform the analysis, we will need copies of your current D&O/E&O policies. We will determine if we can improve the coverage – and maybe even the pricing. Please contact your Summit Re representative to begin the process.


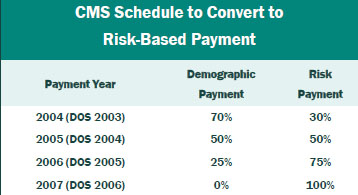
 Beam Partners, LLC specializes in helping healthcare plans recover additional Medicare premium by using custom software that combines your medical claims and pharmacy data to identify the medical records that qualify.
Beam Partners, LLC specializes in helping healthcare plans recover additional Medicare premium by using custom software that combines your medical claims and pharmacy data to identify the medical records that qualify.