Summit Reinsurance Services, Inc. today announced a strategic collaboration with Deerwalk, Inc., an innovative population health management, data management, and healthcare analytics software company. Through this collaboration, Summit Re clients will have access to the most complete population health management suite in the industry. Efficient and accurate data collection, intake, enrichment, and reporting, will allow participating clients to obtain a full picture of their risk portfolio in order to make more effective management decisions.
Read moreTransplantation and Expanded Criteria Donors: Hepatitis C
This shortage of available organs has led to the increased use of Expanded Criteria Donors in transplant centers for many different organs. This article discusses liver transplant recipients who are hepatitis C negative and receive a liver from an expanded criteria liver donor who is Hepatitis C positive.
Read moreSummit ReSources 2018 Outcomes
Summit ReSources helped clients realize more than $30 million in savings for 2018.
Read moreEligibility – Best Practices for Health Insurers
Healthcare reform will continue to require more responsibility from employers – especially small employers – which will, in turn, require more oversight by insurers. If employer groups are not properly enrolling, verifying eligibility, and reporting members, the health plan could find itself at risk with its reinsurer. The best way to avoid potential conflicts is to make sure your master contract is clear – and then to enforce it.
Read moreSummit Moves Forward with Zurich Strategic Alliance
This special edition of Summit Perspectives provides an in-depth explanation of the new Summit Re partnership with Zurich American Insurance Company for catastrophic medical excess of loss business across all product lines.
Read moreAbout Zurich
Zurich Insurance Group (Zurich) is a leading multi-line insurer that serves its customers in global and local markets. With more than 55,000 employees, it provides a wide range of general insurance and life insurance products and services. Zurich’s customers include individuals, small businesses, and mid-sized and large companies, including multinational corporations, in more than 170 countries. The Group is headquartered in Zurich, Switzerland, where it was founded in 1872. The holding company, Zurich Insurance Group Ltd (ZURN), is listed on the SIX Swiss Exchange and has a level I American Depositary Receipt (ZURVY) program, which is traded over-the-counter on OTCQX. Further information about Zurich is available at www.zurich.com. In North America, Zurich is a leading commercial property-casualty insurance provider serving the global corporate, large corporate, middle market, specialties and programs sectors through the individual member companies of Zurich in North America, including Zurich American Insurance Company. Life insurance and disability coverage issued in the United States in all states except New York is issued by Zurich American Life Insurance Company, an Illinois domestic life insurance company. In New York, life insurance and disability coverage is issued by Zurich American Life Insurance Company of New York, a New York domestic life insurance company. For more information about the products and services it offers and people Zurich employs around the world go to www.zurichna.com. 2012 marked Zurich's 100 year anniversary of insuring America and the success of its customers, shareholders and employees.
Zurich Financial Strength
Financial strength ratings (as of September 30, 2014): A.M. Best > A+/Stable
Standard & Poor's > AA-/Stable
Recognition and awards:
Zurich named “Best Insurance Company” (Captive LIVE USA Conference, October 2014)
2014 Innovation Award: “What if?” Zurich Risk Grading™ Application (Business Insurance, March 2014)
Zurich winner of the AGC Community Award (Associated General Contractors of America, Annual Conference, March 2014)
2014 Innovation Showcase: “Zurich Risk Room” and “My Zurich Portal” (Best’s Review magazine, January 2014)
Zurich “Best Political Risk Insurer,” “Best Global Supply Chain/Trade Disruption Insurer,” “Best Property Insurer,” “Best D&O Insurer,” “Best Employment Practices Liability Insurer,” “Best Crime/Fidelity Insurer” and “Best General Liability Insurer” (Global Finance Magazine, October 2013)
Zurich’s Trade Credit and Political Risk group named “Best Private Insurer in Trade,” “Best Trade Insurer in North America,” “Best Trade Insurer in Asia Pacific” and “Best Trade Insurer in Latin America” (Trade Finance, June 2013)
2013 Innovation Award: Zurich Risk Room Mobile Application (Business Insurance, March 2013)
2013 “Innovation in Fronting” Award: UK Captive Services Awards (Captive Review, February 2013)
Zurich named “Best Fronter of the Year” (Captive LIVE USA Conference, September 2012)
Zurich’s Trade Credit and Political Risk group named “Best Private Insurer,” “Best Trade Insurer in Asia Pacific” and “Best Trade Insurer in North America” (Trade Finance, August 2012)
Zurich named “2011 Insurer of the Year” (Daimler Financial Services AG, August 2012)
Innovation Award for Zurich Multinational Insurance Application (Zurich MIA) (Business Insurance, March 2012)
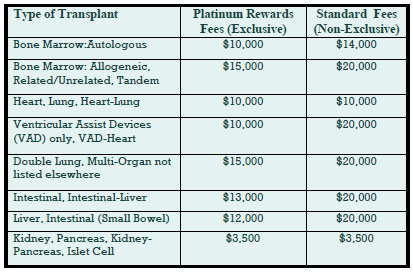
Deep Discounts on Transplant Program Fees
Deeply discounted transplant access fees are available through our new Platinum Rewards program, an enhanced OptumHealth Care Solutions (formerly United Resource Networks) program. This program is available only to Summit Re’s clients. Under our previous program, you received a 5% discount on network access fees, an additional 5% discount if you agreed only to use OptumHealth’s networks, and up to 10% based on Summit Re’s total volume of business with OptumHealth. The third discount was calculated retrospectively.
These three potential discounts are now bundled into one substantial discount. The program is easier to use and easier to understand. You will be able to realize the total savings we've negotiated “up front” through reduced access fees.
The savings from the Platinum Rewards program can be significant, as shown in the chart. Based on our historical case mix, the Platinum Rewards program represents an effective 27% discount off standard OptumHealth fees.
To be eligible for Platinum Rewards, you must agree only to use the OptumHealth networks for your transplants, although you can still “carve out” facilities with which you have your own contracts.
The new program is effective on January 1, 2008. You will need to execute a new Payer Access Agreement, selecting either the fees for the Platinum Rewards program or the standard access fees.
Platinum Rewards Frequently Asked Questions
Which of the OptumHealth programs will be subject to the reduced fees?
The reduced fees apply to the Transplant Resource Services’ Centers of Excellence program and the Transplant Access Program for business that is reinsured through Summit Re. All other OptumHealth program fees remain unchanged.
Do the reduced fees apply to both adult and pediatric transplants?
Yes, the reduced fees apply to adult and pediatric transplants.
How will the Platinum Rewards program affect the OptumHealth transplant facility contracts and services?
The new program has the same facility contracts and services contained under the current OptumHealth programs.
Will I be able to “carve out” a specific facility from the OptumHealth contract and use my own contract at that OptumHealth facility?
You will still have the capability of carving out a facility or facilities from the OptumHealth agreement. Those facilities should be listed on Exhibit C of the Payer Access Agreement.
What happens if I want to use another transplant network in addition to OptumHealth?
You may use another network in addition to OptumHealth. However, if you do so, you will not be eligible for the reduced fees available through the Platinum Rewards program. You will pay OptumHealth’s standard access fees.
What do I need to do to initiate the new program?
If you are currently accessing OptumHealth through Summit Re, you will need to sign a new Payer Access Agreement. New Payer Access Agreements will be mailed to Summit Re clients. Be sure to indicate if you intend to use the OptumHealth network only or if you will use another network in addition to OptumHealth’s network.
Will I still receive this year’s discount based on Summit Re’s total volume of business with OptumHealth?
You will still be eligible for the discount for 2007 based on Summit Re’s total volume of business with OptumHealth, provided you are a Summit Re client at the time the refund is paid. OptumHealth has committed to paying this refund within 60 days after the end of the calendar year.
ERC / Westport Merger
Swiss Re has received regulatory approval to merge Westport Insurance Corporation into Employers Reinsurance Corporation. The merger is an example of Swiss Re’s focus on smart capital management, delivering greater efficiency and reducing operating costs. Reinsurance agreements issued after January 1, 2008 will bear the Westport name. There will be no changes in coverage as a result of the merger. If you have any questions, please contact Summit Re at 260-469-3000.
After the Claims are Paid
This article is part of a series of case studies—real stories of how managed care companies increased profits by using Summit Re’s resources to increase sales, decrease expenses, and manage claims. This case study addresses one of the latest developments in managed care—post-payment administration and claim recovery. Imagine the impact on your bottom line if you recovered 2 to 3 percent of claims, after all current internal processes were completed.
This service is available through Summit Re’s arrangement with Health Decisions, Inc., one of the most comprehensive and sophisticated post-payment administrators in the country. Independent benchmarking analyses have confirmed that its approach sets new standards for the use of data produced by claim payment, enrollment, and related systems. Through its services, you have access to postpayment support equivalent to that available to the largest payers— without development costs or lead time.
Potential recovery areas
The focus for recoveries occurs in the following areas:
- Other liable parties not correctly reported by enrollees for benefit coordination
- Medicare-as-primary payer (ESRD, retirees, disabled) to offset any Medicare-as secondary-payer demands
- Enrollment discrepancies, such as ineligible and terminated members, family status changes, etc.
- Provider billing errors, such as inappropriate service codes, unbundling, duplicate payments, discount avoidance, fee inflation, double billing, etc.
- “Not a covered benefit” enforcement at the procedure code level
- Judicial judgments, such as divorces, workers compensation, and subrogation
Services available
Existing data are combined with new data and converted to Microsoft® compatible files. This new data set has many applications, including supporting internal client management, maximizing claim recovery returns and processing efficiency, and supporting new client service offerings.
Claim Recovery Service
Identifies claims that should have been paid by others and pursues collection from other payers, such as Medicare or insurers, and providers.
Enrollment Support Service
Handles all the details of special (non-routine) employee/enrollee communications to compile, compare and reconcile internal and external data files across multiple payers.
Recovery Software
Use of Health Decisions, Inc.’s proprietary software on internal network systems.
Data Support Services
A full range of technical support permits translation of any documented file structure into Microsoft® compatible files for HIPAA compliant data analysis, reporting and warehousing.
Flexible payment arrangements
Health Decisions, Inc. can be compensated on a contingency basis, keeping 33% of recovered claim amounts. Health Decisions, Inc. is also willing to enter into a multiyear, fixed-fee software lease covering its Paperless Claim Recovery software suite and all related support services.
Client results
Client “A” used post-payment findings to pursue claim recovery and returned $15 per member per year to its bottom line.
Client “B” used post-payment findings as a continuous-quality improvement management tool to monitor internal performance improvements.
Client “C” used post-payment findings to pinpoint “problem” providers and to support provider contracting negotiations.
Health Decisions, Inc.
Health Decisions, Inc. is an established, reputable and successful post-payment administration and claim recovery vendor. In one yearalone, they processed almost two billion dollars of paid claims. In the area of claim recovery, nobody addresses more recovery areas (40+ review areas), offers a lower recovery threshold (all claims over $10) or recovers a greater amount of money per client (2-3 percent of claims).