As a result of the survey and client conversations, the following Summit ReSources portfolio of services was structured. Each vendor underwent a stringent due diligence process. An onsite visit to the primary facility providing the service was part of the process for the majority of the vendors. If you would like to learn more about any of the programs or have any questions, please contact Debbie Stubbs or Laura Pearce. If there are other programs you think we should consider adding to Summit ReSources, please let us know. Transplant Management
United Resource Networks (URN)
URN offers consulting expertise and access to over 100 of the nation's most prestigious medical centers specializing in organ and tissue transplantation. Specialized Physician Review services are also available, whereby our customers can obtain independent, expert medical opinions of the appropriateness of proposed transplants for specific members and in the area of congenital heart disease.
URN also has a Congenital HeartDisease program, which includes access to a network of facilities that excel in the treatment of congenital heart disease (CHD). The CHD programs complement the heart transplant expertise found within the URN transplant network.
Claim Recovery
Health Decisions, Inc. (HDI)
HDI specializes in benefit management services that produce a 3:1 return on investment within 12 months, while leaving current coverage intact. HDI provides claim recovery and enrollment support services.
Disease Management
See related article (click here).
National PPO Network
GlobalCare, Inc.
By offering access to a 24-hours-a-day, 7-days-a-week Medical Help Desk, as well as through relationships with over 100 PPO networks andnegotiators, GlobalCare allows your members to have medical assistance and network access anywhere in the United States and around the world.
Predictive Modeling
Integrated Healthcare Information Services, Inc. (IHCIS)
Impact Pro is IHCIS’s industry-leading, rules-based predictive modeling tool that produces a measure of future relative risk, a prediction of future health care costs, relative risk for an inpatient admission and the probability of one or more admissions for each enrolled member of a health plan. These measures of risk can be used in medical management and have financial, actuarial and underwriting applications. Impact Pro is used by leading health plans and clinicians across the United States, serving more than 30 million Americans.
Non-Network Claims Management
Global Claim Services (GCS)
GCS specializes in clinical and financial claims reviews, offering a personalized, process-oriented approach for out-of-network medical claims and fee negotiations for inpatient and out-patient facilities, professional services and ancillary fees.
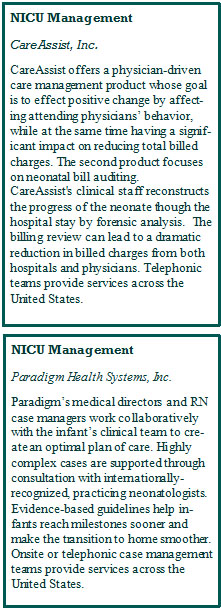
Neonatal Intensive Care Management
See related article (click here).
Catastrophic Illness and Injury
Paradigm Health Systems, Inc,
The highly skilled staff specializes in management of a variety of catastrophic medical events, such as brain injuries, spinal cord injuries, complex burns and severe trauma.