Neonatal Trends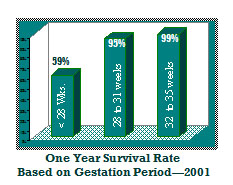 In 2002, the rate of preterm births was reported as 12.1% of all births, and prematurity was the leading cause of neonatal mortality and birth-related morbidity. Preterm birth is defined as birth before 37 weeks of completed gestation. Due to the rising rate of multiple births, the proportion of preterm infants has increased by 14% since 1990.
In 2002, the rate of preterm births was reported as 12.1% of all births, and prematurity was the leading cause of neonatal mortality and birth-related morbidity. Preterm birth is defined as birth before 37 weeks of completed gestation. Due to the rising rate of multiple births, the proportion of preterm infants has increased by 14% since 1990.
In the 1970s, infants born at a gestational age of 28 weeks were considered extremely premature. Today, some infants born at 21-22 weeks are able to survive. The low birth weight rate (less than 2,500 grams) increased to 7.8% in 2002, the highest level reported in more than three decades. The rate of very low birth weight infants (less than 1,500 grams) was 1.46% in 2002.
The twin birth rate continued to climb, at 31.1 per 1,000 births in 2002. This represents an increase of 38% since 1990 and a 65% increase since 1980. The rate of triplet and higher-order multiple births declined slightly in 2002. However, there was an overall increase in these higher-order multiple births of more than 400% between 1980 and 1998. This increase was attributed to advances in and greater access to fertility therapies and to childbearing at older ages. Women in their thirties are more likely to have multiple births than younger women, even without fertility treatment.
Complications and Medical Problems
Due to the advances in NICU management and technology, babies are being born earlier and are surviving, but not without complications and medical problems. The most common problems include respiratory distress syndrome, patent ductus arteriosis, apnea of prematurity, intraventricular hemorrhage, necrotizing enterocolitis, retinopathy of prematurity, sepsis, and bronchpulmonary dysplasia. Nearly half of all long-term, congenital neurological defects are due to prematurity.
Medical Care and Associated Cost
The annual cost of prematurity to employers' health plans, which included the cost to the employer and employee, was estimated at $4.7 billion in 1992. The federal-state Medicaid program finances 3% of births nationally. 2 NICU care is generally separated into four levels, with Level I providing care for uncomplicated obstetrical and neonatal populations and Level IV managing the most complicated patients. Hospital facilities define the levels differently, so it is prudent to ask the facility what types of services are provided in each level and by what type of healthcare providers. Level IV NICUs are often hectic, noisy places. This environment may contribute to the physiologic instability of the infants and may interfere with recovery from illness, growth and development. Infants may manifest signs of stress by changes in skin color (mottling), apnea, bradycardia, hiccups, posturing and reflux of feedings. NICUs are now moving toward providing care while trying to decrease the effects of the environment. Measures may include darker rooms, covers for isolettes, soft music, scheduling care in clustered blocks of time to allow rest periods, swaddling, positioning aids, and occupational/physical therapy to work on developmental milestones.
Sources:
- National Vital Statistics Reports, Vol. 52, No. 10, Dec. 17, 2003.
- National Center for Health Statistics, final natality data for 2000. Prepared by March of Dimes Perinatal Data Center, 2002.
- Hazinski, MF (1999). Manual of Pediatric Critical Care.